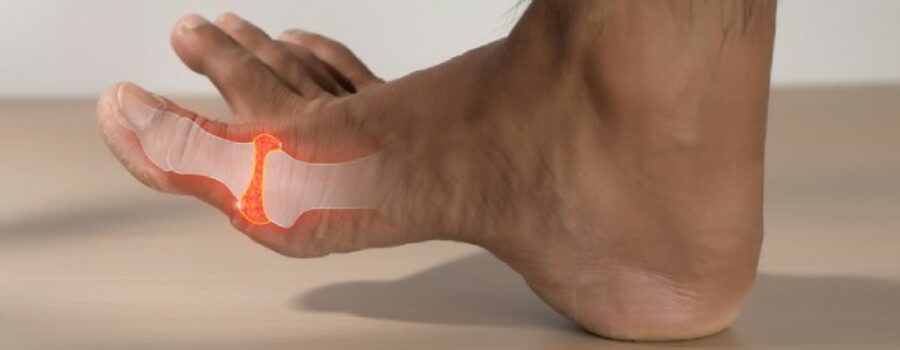
Imagine waking up in the middle of the night with an intense, burning pain in your big toe. The joint is swollen, red, and feels like it’s on fire. This excruciating scenario is all too familiar for those suffering from gout, a complex form of arthritis that primarily affects the feet.
But what causes gout in feet, and how can it be managed or prevented?
Understanding the factors behind this condition is essential for anyone who wants to avoid the painful flare-ups associated with gout. In this article, we’ll delve into the causes of gout, identify foods and drinks that can trigger attacks, and provide practical tips for managing and preventing this condition.
Let’s explore the ins and outs of gout, starting with what it is and who’s most affected.
What Is Gout?
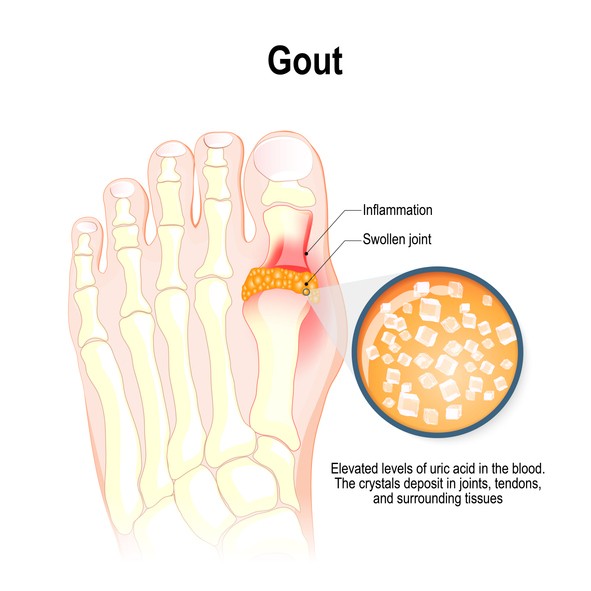
Gout is a form of arthritis characterized by sudden and severe pain, redness, and swelling in the joints.
The Arthritis Society of Canada explains that gout occurs when uric acid accumulates in the blood for an extended period of time. This leads to the formation of sharp crystals in a joint or surrounding tissue. These crystals cause intense inflammation and pain, which is why gout attacks can be so debilitating.
Although gout can affect any joint, it most commonly targets the feet, particularly the big toe. The symptoms often appear suddenly, usually at night, and can persist for days or even weeks.
Gout has been historically known as the “disease of kings” because it was thought to be caused by a diet rich in meats and alcohol—luxuries that were once accessible only to the wealthy.
Today, we understand that gout can affect anyone, and while diet plays a role, it’s far from the only factor involved.
Who’s Affected by Gout?
According to the Arthritis Society of Canada, an estimated 1 million Canadians have gout, making it the most common form of inflammatory arthritis. Additionally, they state that men are more often affected than women, with roughly 4% of men having gout as opposed to 1% of women.
Gout does not discriminate by age, but it most commonly affects men aged 30 to 50. When it comes to women and gout, they are more likely to develop this condition after menopause, likely due to a drop in estrogen levels, which helps keep uric acid levels in check.
Individuals with a family history of gout are also at a higher risk, as are those with certain health conditions such as obesity, hypertension, or kidney disease. Additionally, lifestyle factors, including diet and alcohol consumption, can significantly increase the risk of developing gout.
Furthermore, gout is more prevalent in populations with diets high in purine-rich foods, such as red meat and seafood.
The condition is also associated with metabolic syndrome, a cluster of conditions including high blood pressure, high blood sugar, and abnormal cholesterol levels, all of which increase the risk of heart disease, stroke, and diabetes.
Given these associations, it’s essential for anyone at risk to understand how lifestyle choices can influence their likelihood of developing gout.
5 Symptoms of Gout in Feet
Gout can manifest in several ways, particularly in the feet. Understanding the symptoms of this condition is crucial for early detection and treatment, which can help prevent long-term joint damage.
1. Severe Joint Pain
The hallmark symptom of gout is intense joint pain, often starting in the big toe. The pain usually begins suddenly and can become so severe that even the weight of a bed sheet can be unbearable. This pain often peaks within 12 to 24 hours and can last for several days or even weeks.
2. Inflammation and Redness
During a gout attack, the affected joint may become visibly inflamed, with noticeable redness and swelling. The area around the joint may feel warm to the touch, and the skin can appear shiny due to the swelling.
3. Stiffness & Swelling
Gout can cause significant stiffness and swelling in the affected joint, making it difficult to move. The joint may feel tender and stiff, particularly after periods of inactivity, such as first thing in the morning.
4. Burning Sensation
A less common but equally uncomfortable symptom is a burning sensation in the joint. This burning feeling often accompanies the intense pain and can make the affected area feel as though it’s on fire.
5. Limited Range of Motion
As gout progresses, the range of motion in the affected joint may become limited. This restriction can make it difficult to walk or perform everyday activities, significantly impacting a person’s quality of life. Over time, repeated gout attacks can lead to chronic arthritis, permanently damaging the joint.
What Causes Gout in Feet & Risk Factors
Understanding what causes gout in feet is key to managing and preventing this painful condition.
Several factors contribute to the development of gout, many of which are modifiable through lifestyle changes. The most predominant risk factors of gout, according to Mayo Clinic, include:
- Obesity, High Blood Pressure, or Diabetes: These conditions are closely linked to the development of gout. Obesity increases the body’s production of uric acid, while high blood pressure and diabetes can interfere with the kidneys’ ability to excrete it. Managing these conditions through diet, exercise, and medication can significantly reduce the risk of gout.
- Kidney Problems: The kidneys play a crucial role in filtering uric acid from the blood. When the kidneys are not functioning properly, uric acid can build up, leading to gout. Individuals with chronic kidney disease are particularly at risk and should work closely with their healthcare provider to monitor and manage uric acid levels.
- Family History of Gout: Genetics play a role in the development of gout. If you have a family history of gout, you are more likely to develop the condition. This hereditary component is why some people develop gout even if they follow a healthy lifestyle.
- Certain Medications: Medications such as diuretics, used to treat high blood pressure, and cyclosporine, an immunosuppressant, can increase uric acid levels in the blood. If you are taking these medications, it is important to discuss the potential risk of gout with your healthcare provider.
- Diet (Certain Foods and Drinks): A diet high in purine-rich foods, such as red meat, organ meat, and certain types of seafood, can lead to increased uric acid levels. Additionally, sugary drinks, alcohol, especially beer, and foods high in fructose can exacerbate the condition. Modifying your diet to avoid these triggers can help manage and prevent gout.

5 Foods & Drinks to Avoid – Preventing Gout
Diet plays a significant role in managing gout. Certain foods and drinks can trigger gout attacks by increasing uric acid levels. Here are five key items to avoid if you’re prone to gout.
1. Red Meat and Organ Meat
These meats are high in purines, which the body breaks down into uric acid. Avoiding red meat, such as beef, lamb, and pork, as well as organ meats like liver and kidneys, can help reduce the frequency and severity of gout attacks.
2. Certain Seafood
Some types of seafood, including anchovies, sardines, mussels, scallops, trout, and tuna, are also high in purines. While seafood is generally considered healthy, individuals with gout should limit their intake of these specific types to prevent flare-ups.
3. Sugary Drinks and Sweets
Fructose, a type of sugar found in many soft drinks and sweets, can increase uric acid production. Avoiding sugary beverages and limiting sweets is not only beneficial for managing gout but also for overall health.
4. Foods High in Fructose and Carbohydrates
Furthermore, fructose-rich foods and refined carbohydrates, such as white bread, pastries, and many processed foods, can contribute to high uric acid levels. Opting for whole grains and reducing intake of sugary foods can help manage gout symptoms.
5. Alcohol
Alcohol is a major contributor to gout, particularly beer, which is high in purines. Even wine and spirits can increase uric acid levels and should be consumed with caution or avoided altogether by those prone to gout.
How Is Gout Diagnosed?
Proper diagnosis is essential for effective gout treatment. If you suspect you have gout, your healthcare provider will likely perform a combination of physical examinations and tests to confirm the diagnosis.
- Physical Exam by Your Healthcare Provider: During a physical exam, your healthcare provider will check for signs of inflammation, swelling, and tenderness in the affected joint. They may also ask about your symptoms and medical history to assess your risk factors for gout.
- Tests (X-rays, Ultrasound, MRI, CT): Imaging tests such as X-rays, ultrasounds, and MRIs can help detect urate crystals in the joints or to rule out other conditions that may be causing your symptoms. These tests provide detailed images of the affected joints, helping healthcare providers to make an accurate diagnosis.
- Other Common Tests (Blood Test, Joint Aspiration): Blood tests can measure the levels of uric acid in your blood, although elevated levels alone do not confirm gout. A more definitive test involves joint aspiration, where a small sample of fluid is taken from the affected joint and examined under a microscope for urate crystals. This procedure is often used to confirm a gout diagnosis and rule out other types of arthritis.
How Is Gout Treated? Common Gout Medication
Gout treatment focuses on relieving pain during attacks and preventing future episodes. Several medications are commonly used to manage gout.
NSAIDs (Ibuprofen, Naproxen, Indomethacin, Celecoxib)
Nonsteroidal anti-inflammatory drugs (NSAIDs) are often the first line of treatment for gout. They help reduce inflammation and relieve pain.
Common over-the-counter NSAIDs include ibuprofen and naproxen, while indomethacin and celecoxib are prescription options. It’s important to take these medications as directed to minimize side effects.
For high-quality affordable over-the-counter NSAIDS, look for the Option+ logo on Health For Your Everyday pain relief products at your local PharmaChoice pharmacy.
Colchicine
Colchicine is another medication used to treat acute gout attacks. It works by reducing the inflammatory response to urate crystals.
While effective, colchicine can have side effects, including gastrointestinal issues, so it’s important to use it under the guidance of a healthcare provider.
Corticosteroids
Corticosteroids, such as prednisone, can be prescribed to reduce inflammation and pain during a gout attack.
They are usually prescribed for short-term use, especially in individuals who cannot take NSAIDs or colchicine. However, long-term use of corticosteroids can have significant side effects, so they are typically reserved for severe cases.
Gout Prevention – Dos and Don’ts
Preventing gout is largely about managing risk factors through lifestyle changes. Here are some easy do’s and don’ts to follow if you’re at risk of developing gout.
DO’s
- Lose some weight if you are overweight
- Drink plenty of fluids (water)
- Exercise regularly
- Eat a healthy diet
DON’Ts
- Drink alcohol
- Drink sugary drinks
- Eat lots of fatty foods or red meats
- Smoke
Adopting these practices can help reduce your risk of gout attacks. For example, losing weight can lower uric acid levels, while staying hydrated helps your kidneys flush out excess uric acid.
On the other hand, avoiding alcohol, sugary drinks, and fatty foods can prevent the buildup of uric acid in the blood.
What Questions Should I Ask My Doctor?
When dealing with gout, it’s essential to have open communication with your healthcare provider. Here are some questions you might consider asking:
What are the possible causes of my symptoms?
Understanding what triggers your gout attacks can help you manage the condition more effectively.
What tests do you recommend?
Ask your doctor about the specific tests that can confirm gout and help rule out other conditions.
Should I see a specialist?
In some cases, it might be beneficial to see a rheumatologist, a specialist in arthritis and related conditions, for further evaluation and treatment.
 Back to myNiagaraOnline
Back to myNiagaraOnline