Plantar fasciitis is a common and often debilitating condition that affects the heel and foot. If you’ve ever experienced sharp, stabbing pain in your heel, especially with those first steps in the morning, you know how disruptive plantar fasciitis can be.
This article delves into plantar fasciitis, offering valuable insights into its causes, symptoms, and diagnosis. We’ll also explore various plantar fasciitis treatments, including the best exercises and stretches to alleviate the pain.
Understanding and addressing this condition effectively can significantly improve your quality of life.
What Is Plantar Fasciitis?
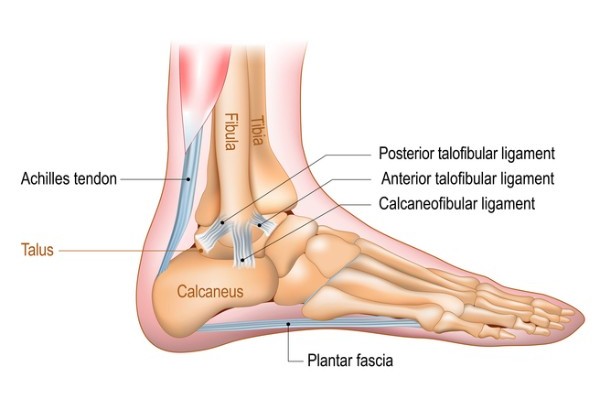
Plantar fasciitis is a condition characterized by inflammation of the plantar fascia, a thick band of tissue that runs along the bottom of your foot, connecting your heel bone to your toes.
The plantar fascia acts like a shock absorber, supporting the arch of your foot and absorbing the impact of activities such as walking, running, and standing.
When this tissue becomes inflamed, it can cause intense heel pain and discomfort, making everyday activities challenging.
What Causes Plantar Fasciitis?
Plantar fasciitis is primarily caused by repetitive strain or overuse of the plantar fascia. Activities that put significant pressure on your heel and the attached tissue can lead to small tears in the fascia, resulting in inflammation and pain.
Common causes include prolonged standing, walking, or running, especially on hard surfaces, as well as wearing unsupportive footwear.
Additionally, sudden increases in activity levels, improper exercise techniques, or engaging in high-impact sports without adequate warm-up and stretching can also contribute to the development of plantar fasciitis.
Certain foot structures, such as flat feet or high arches, can predispose individuals to this condition by placing extra stress on the plantar fascia.
What Does Plantar Fasciitis Feel Like?
Individuals with plantar fasciitis typically experience the following symptoms:
- Sharp, stabbing pain: This pain is most commonly felt at the bottom of the heel.
- Morning pain: Pain is often most severe with the first steps taken in the morning.
- Pain after inactivity: Discomfort can return after periods of rest or inactivity.
- Worsening pain with activity: Prolonged standing, walking, or physical activity can exacerbate the pain.
- Pain after exercise: Intense pain may occur after, not during, physical activity.
These symptoms can significantly impact daily activities and quality of life.
How Common Is Plantar Fasciitis?
Plantar fasciitis is quite common, affecting millions of people each year. It is particularly prevalent among athletes, runners, and individuals who spend long hours on their feet.
According to the Pedorthic Association of Canada, plantar fasciitis affects roughly 10% of Canadians at some point in their lives and accounts for about 80% of complaints regarding heel pain.
It is particularly prevalent among athletes, runners, and individuals who spend long hours on their feet.
The high incidence rate underscores the importance of understanding and managing this condition effectively to prevent long-term discomfort and disability.
What Are the Risk Factors for Plantar Fasciitis?
Certain factors can significantly increase your risk of developing plantar fasciitis, such as:
- Age: According to Mayo Clinic, people between the ages of 40 and 60 are most likely to develop this condition.
- High-impact exercise: Activities like running, ballet, or demanding sports can result in an increased risk for plantar fasciitis.
- Weight: The more pressure your feet experience, the higher your risk of developing this condition. Obesity significantly increases the stress on the plantar fascia, resulting in a higher potential for occurrence.
- Foot mechanics: The shape of your foot, such as flat feet or high arches, or your walking pattern can impact the risk of your developing plantar fasciitis. This includes factors like the height of your arch or the way weight is distributed on your feet as you walk.
- Your occupation: Jobs that involve long hours on your feet, such as teaching or factory work, can lead to plantar fasciitis.
Understanding these risk factors can help in taking preventive measures to avoid plantar fasciitis.
Plantar Fasciitis Symptoms
The symptoms of plantar fasciitis can vary in intensity and duration but often include:
- Heel pain: This is the most common symptom and is described as sharp, stabbing pain in the bottom of the heel. It is usually most intense with the first steps after waking up in the morning or after periods of rest.
- Stiffness: Individuals often experience stiffness in the heel and foot, particularly after periods of inactivity, making it difficult to walk or move comfortably.
- Pain in the foot arch: Discomfort can extend into the arch of the foot, causing a more widespread ache.
- Swelling around the heel: Inflammation and swelling may occur near the heel area, adding to the discomfort and pain. This swelling is a result of the ongoing inflammation in the plantar fascia.
Plantar Fasciitis Diagnosis – How It Can Be Diagnosed?
Early diagnosis accurately is crucial for effective plantar fasciitis treatment. The diagnostic process typically involves a combination of a physical examination and imaging tests to confirm the condition and rule out other potential causes of heel pain.
Physical Exam:
During the physical exam, your healthcare provider will look for areas of tenderness in your foot, specifically in the heel and along the plantar fascia.
The location and intensity of the pain can provide valuable clues. Your provider may ask you to flex your foot while pressing on the plantar fascia to see if the pain intensifies, helping to pinpoint the inflammation’s source.
Imaging Tests:
Although not always necessary, imaging tests can be useful in diagnosing plantar fasciitis and ruling out other conditions.
X-rays can reveal bone spurs or fractures, while MRI scans provide detailed images of soft tissues.
Alternatively, your healthcare provider may request an ultrasound. This offers real-time imaging and is useful for evaluating soft tissue structures.
These tests can show signs of inflammation or tears in the plantar fascia, confirming the diagnosis.
A thorough diagnosis involving both a physical exam and, if needed, imaging tests ensures that the appropriate treatment plan is developed. Proper diagnosis is the first step toward relieving the pain and discomfort associated with plantar fasciitis and preventing future episodes.

Plantar Fasciitis Treatment – How It Can Be Treated?
Treating plantar fasciitis involves a combination of self-care measures and medical interventions to relieve pain and promote healing.
Home Remedies
Several self-care measures can help alleviate the symptoms of plantar fasciitis and support the healing process:
- Resting: Reducing or avoiding activities that exacerbate the pain can significantly decrease inflammation and allow the plantar fascia to heal.
- Icing Your Foot: Apply ice to the affected area for 10 minutes on and 10 minutes off, particularly after being active. This can be done several times a day as needed to help reduce pain and inflammation.
- Massaging and Stretching: Regularly massaging and stretching the foot and calf muscles can alleviate tension, improve circulation, and enhance flexibility. These exercises can be easily incorporated into your daily routine.
- Orthotics, Supportive Shoes, or Shoe Inserts: Using custom orthotics or over-the-counter shoe inserts can provide additional support and cushioning, helping to redistribute pressure on the feet. Wearing shoes with good arch support and a cushioned sole can also make a significant difference.
- NSAIDs (Nonsteroidal anti-inflammatory drugs): Tylenol (Acetaminophen), Advil (ibuprofen), or Aleve (naproxen) can help manage pain and reduce inflammation.
Medical Interventions
When home remedies are not sufficient, medical interventions may be necessary:
- Physical Therapy: A physical therapist can guide you through exercises and stretches that strengthen the muscles and ligaments in your foot, improving flexibility and reducing strain on the plantar fascia.
- Immobilization: In severe cases, immobilizing the foot with night splints, a walking boot or a brace may be necessary to allow the plantar fascia to heal properly and prevent further strain.
- Medical Procedures: In rare instances where conservative treatments fail, surgical interventions may be considered. As explained by Mayo Clinic, these can include injections (such as corticosteroids to reduce inflammation), shock wave therapy, ultrasonic tissue repair or even surgery to release the plantar fascia and relieve tension.
By combining these approaches, patients can effectively manage and eventually overcome the symptoms of plantar fasciitis.
Plantar Fasciitis Prevention – How Can I Prevent It?
Preventing plantar fasciitis involves taking proactive steps to reduce strain on your feet and maintain overall foot health. Here are some effective strategies:
- Wear Supportive Shoes: Choose shoes with good arch support and cushioning to reduce stress on your feet. Proper footwear can significantly reduce the risk of plantar fasciitis, especially if you spend long hours standing or walking.
- Rest Your Feet After Physical Activity: Allow time for your feet to recover after strenuous activities. Avoid overuse by incorporating rest periods into your routine, particularly after high-impact exercises.
- Regular Stretches: Incorporate stretches before and after exercise to maintain flexibility and strength in your foot and calf muscles. Stretching helps prevent the buildup of tension in the plantar fascia, reducing the likelihood of injury.
- Replace Your Sneakers Every Few Months: Often, athletes develop foot problems because their shoes are worn out or no longer fit properly. Ensure your footwear is in good condition and provides adequate support. Worn-out shoes lose their cushioning as padding wears out, and the tread or heels wear down, affecting the shoe’s support structure.
- Maintain a Healthy Weight: This can help reduce the load on your feet. Excess weight puts additional strain on the plantar fascia, increasing the risk of developing plantar fasciitis. A balanced diet and regular exercise can help maintain a healthy weight and alleviate foot stress.
By following these preventive measures, you can minimize the risk of developing plantar fasciitis and maintain healthier, pain-free feet.

7 Best Exercises & Stretches for Plantar Fasciitis
Engaging in specific exercises and stretches can help alleviate the symptoms of plantar fasciitis and prevent its recurrence. Here are detailed instructions for each stretch:
Stair Stretches:
- Stand on a step with your heels hanging off the edge.
- Hold onto a railing for balance.
- Slowly lower your heels below the step level until you feel a stretch in your calves and plantar fascia.
- Hold for 15-30 seconds, then return to the starting position.
- Repeat 3 times.
Wall Stretches:
- Stand facing a wall with your hands placed on the wall at shoulder height.
- Step one foot back, keeping it straight, while bending the front knee.
- Press your back heel into the ground.
- Hold the stretch for 15-30 seconds.
- Switch legs and repeat 3 times per leg.
Calf Stretch:
- Sit on the floor with your legs extended in front of you.
- Wrap a towel around the ball of your foot.
- Gently pull the towel toward you, keeping your leg straight.
- Hold for 15-30 seconds.
- Repeat 3 times per leg.
Rolling Stretch:
- Sit in a chair and place a tennis ball or frozen water bottle under your foot.
- Roll the object back and forth under your arch for 1-2 minutes.
- Apply gentle pressure as needed.
Towel Curls:
- Sit on a chair and place a towel on the floor in front of you.
- Use your toes to scrunch the towel and pull it toward you.
- Repeat the motion for 1-2 minutes per foot.
Seated Foot Stretch:
- Sit with one leg crossed over the other.
- Gently pull back on the toes of the crossed leg until you feel a stretch in the arch of your foot.
- Hold for 15-30 seconds.
- Repeat 3 times per foot.
Marble Pickups:
- Place several marbles on the floor.
- Use your toes to pick up the marbles one by one and place them in a cup.
- Continue for 1-2 minutes per foot.
Incorporating these exercises and stretches into your daily routine can help manage plantar fasciitis symptoms and prevent future occurrences.
When to Call a Doctor
Knowing when to seek professional medical advice is crucial for managing plantar fasciitis effectively.
- Your Pain Doesn’t Go Away After a Week: Persistent pain that does not improve with self-care measures warrants a visit to your healthcare provider.
- The Symptoms Don’t Improve After 2 Weeks of the Treatment: If there is no significant improvement after two weeks of treatment, consult your healthcare provider for further evaluation.
Prior to your appointment, prepare a list of questions to discuss with your healthcare provider, such as potential treatment options, exercises, and preventive measures.
 Back to myNiagaraOnline
Back to myNiagaraOnline